
The coronavirus epidemic continues to have a significant impact on our everyday lives, infecting hundreds of thousands of individuals each week. COVID-19 rapid antigen tests are a very effective method of protecting yourself and your family. However, which exam is appropriate for you? Dr. Christopher Carpenter, a Beaumont infectious disease specialist and chair of internal medicine, has the answers.
What are the many COVID-19 test types?
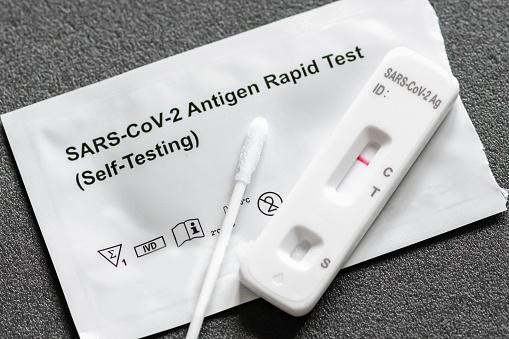
There are two primary kinds of COVID-19 rapid antigen tests available at the moment.
- Viral testing may be used to determine whether a person is currently infected with COVID-19. Nucleic acid amplification rapid antigen tests (NAATs) and antigen testing are two frequent forms of viral diagnostics. You may have heard NAATs referred to as polymerase chain reaction (PCR) testing. Vaccination will not result in a positive result on these rapid antigen tests.
- Antibody rapid antigen tests, often called serology tests, may determine whether you have ever been infected with the coronavirus, but they cannot identify an active infection. Depending on the antibody target (i.e., those directed against the spike protein), this test may potentially detect a response to past immunization in an individual who has never been sick.
While certain viral tests may be performed on-site or even at home, others must be transported to a laboratory for processing.
“While on-site testing is convenient and produces findings quickly, it has significant limits,” Dr. Carpenter said. “In many circumstances, operators are restricted in their ability to complete a particular number of rapid antigen tests within a certain amount of time. Sensitivity and precision might sometimes be a problem.”
While laboratory tests are more precise, they may take longer to complete.
Which Examination Should You Take?
“Which test is best for you is situation-dependent,” Dr. Carpenter said. “Some rapid antigen tests are only authorized for persons who are already experiencing symptoms, and they should not be used for screening if you are feeling well. The best test is one that provides the most accurate result in the shortest amount of time.”
When time is critical, an antigen or fast test may be the best option. Numerous rapid antigen tests are now accessible as home test kits, which eliminates the need to visit a health care institution. If you have the patience to await the findings of a laboratory-based test, you will often obtain the most accurate results. learn more about rapid antigen tests by clicking here.
While no test is perfect, the ones now available are very accurate when done properly. If you choose an at-home test, it is critical to carefully follow the directions for the best results. Individuals who continue to suffer symptoms after a negative COVID-19 test may seek repeat testing.
When should you get tested for COVID-19?
COVID-19 rapid antigen tests are beneficial for confirming or ruling out an infection, particularly as we approach flu season. Not only may the outcome impact treatment choices, but it can also assist safeguard individuals in your immediate vicinity. learn more about clinical supplies at https://clinicalsupplies.com.au/
The CDC advises that everyone who exhibits symptoms consistent with COVID-19 be tested, even those who are completely vaccinated or have been infected before. Additionally, those who have not been vaccinated but have traveled, attended big meetings, or been in poorly ventilated interior settings should be examined.
Individuals who have been completely vaccinated and have been exposed to someone who has COVID-19 should seek rapid antigen tests to confirm they have not caught the virus. While the individual may be symptom-free, they may still transmit the illness to others. If positive, rapid antigen tests assist in preventing this with adequate isolation.
- If you feel you have been exposed to COVID-19 and are completely vaccinated, you should test 5-7 days following your original exposure.
- If you believe you have been exposed to COVID-19 but are not fully vaccinated, you should test immediately. If your test result is negative, be certain to retest (5-7 days after the initial exposure or immediately after symptoms develop).
Anyone wanting to go overseas or returning to the United States after an international trip may be needed to have a recent negative COVID-19 test. Because specific restrictions vary per location, it is important to verify and make the necessary preparations before visiting.
How to safeguard oneself while awaiting test results
“If you are asymptomatic and undergoing regular rapid antigen tests, such as before to travel, there are no restrictions other than the advised precautions,” Dr. Carpenter says.
Individuals who have not been vaccinated and have been exposed to COVID-19 should consider self-quarantine. Individuals who have been vaccinated may not be required to quarantine, but they should check themselves for signs and continue to take measures. The CDC advises isolation for anybody exhibiting COVID-19 symptoms while awaiting test results.
Despite extensive rapid antigen tests, Dr. Carpenter underlines that immunization remains the most effective method of preventing COVID-19.
Investigating genetic evidence
For any kind of test, the initial step is to get a sample from the patient. This might be a swab of the nose or a little amount of saliva.
For PCR rapid antigen tests, the following step is an amplification of the genetic material, which allows for detection of even a minute quantity of coronavirus genes in the patient’s sample. This is accomplished via the use of a process known as a polymerase chain reaction. A health care professional collects the sample and uses an enzyme to convert it to double-stranded DNA.
The DNA is then heated in the presence of a solution containing an enzyme called a polymerase, causing it to split into two single-stranded DNA fragments. The temperature is dropped, and polymerase attaches to and replicates the single-stranded DNA with the assistance of a short bit of guide DNA called a primer. The primers are designed to amplify just coronavirus DNA. You have now replicated coronavirus DNA twice from the initial RNA fragment.
Laboratory machinery performs these heating and cooling cycles 30–40 times, doubling the DNA to a billion copies. The amplified sequence is labeled with a fluorescent dye that allows it to be read by a machine.
Due to the amplification ability of PCR, even the tiniest quantity of coronavirus genetic material in a sample may be detected effectively. As a result, it is a very sensitive and accurate test. It is the gold standard for diagnosing SARS–CoV–2 because of its near-perfect accuracy.
However, PCR rapid antigen tests have several limitations. They need a trained laboratory operator and specialized equipment to operate, and the whole amplification process might take an hour or more. Generally, only big, centralized rapid antigen tests facilities – such as hospital laboratories – are capable of performing several PCR rapid antigen tests concurrently. Between sample collection, transportation, amplification, detection, and reporting, a person should expect to wait between 12 hours and five days for findings. Finally, they are not inexpensive, costing $100 or more each test.